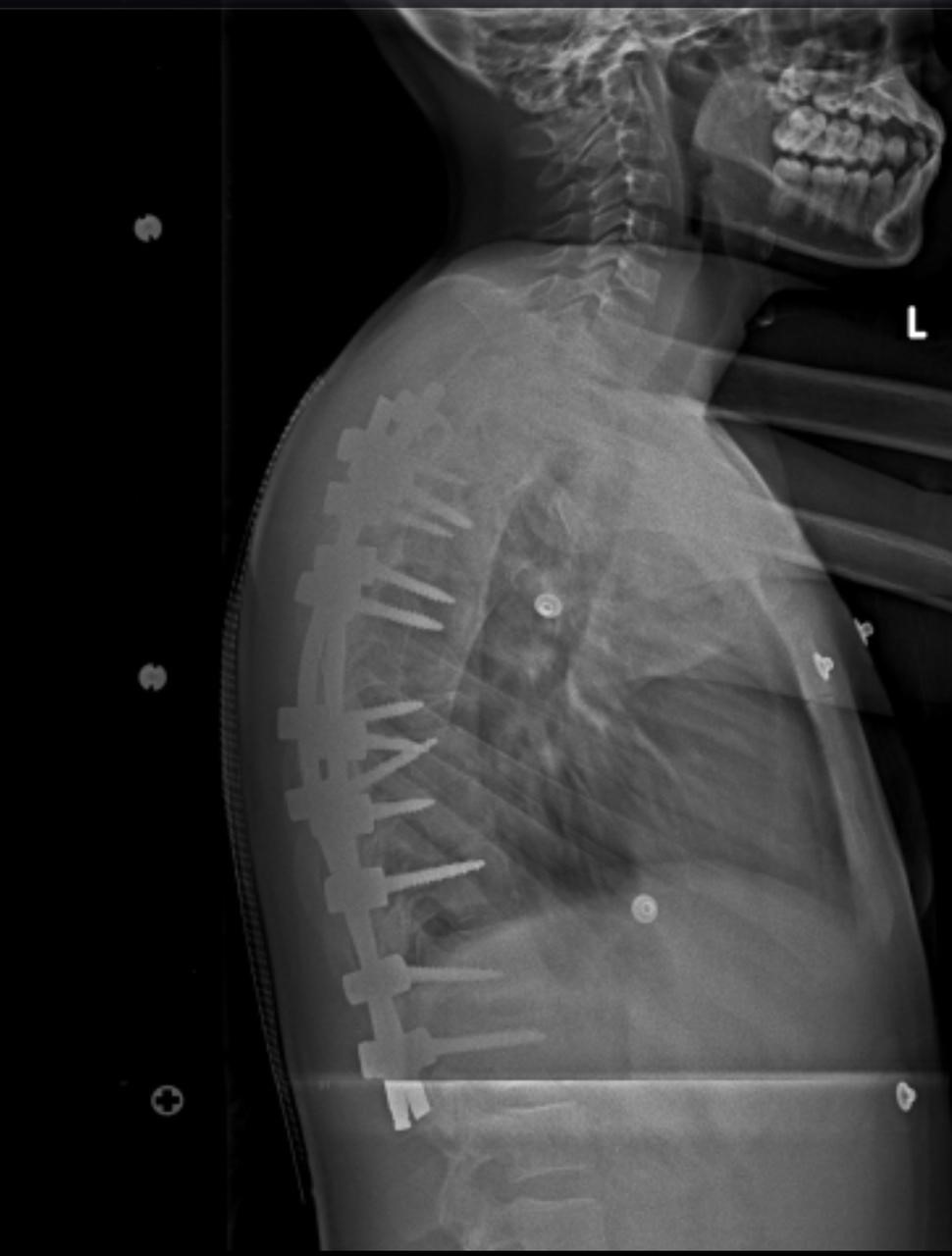
Haemorrhagic Stroke
What is haemorrhagic stroke?
A haemorrhagic stroke happens when blood from an artery bleeds into the brain after a blood vessel bursts.
What causes haemorrhagic stroke?
- Uncontrolled high blood pressure
- Overtreatment with blood thinners (anticoagulants)
- Bulges at weak spots in your blood vessel walls (aneurysms)
- Protein deposits in blood vessel walls that lead to weakness in the vessel wall (cerebral amyloid angiopathy)
- Ischemic stroke leading to hemorrhage (infarct with haemorrhagic transformation)
The warning signs of stroke are:
- Sudden onset of weakness or numbness on one side of the body.
- Sudden speech difficulty
- Sudden difficulty seeing in one or both eyes or double vision(diplopia)
- Sudden onset of dizziness, trouble walking or loss of balance.
- Sudden, severe headache with no known cause
However, symptoms can vary based on the location of the haemorrhage in the brain.
Management of haemorrhagic stroke
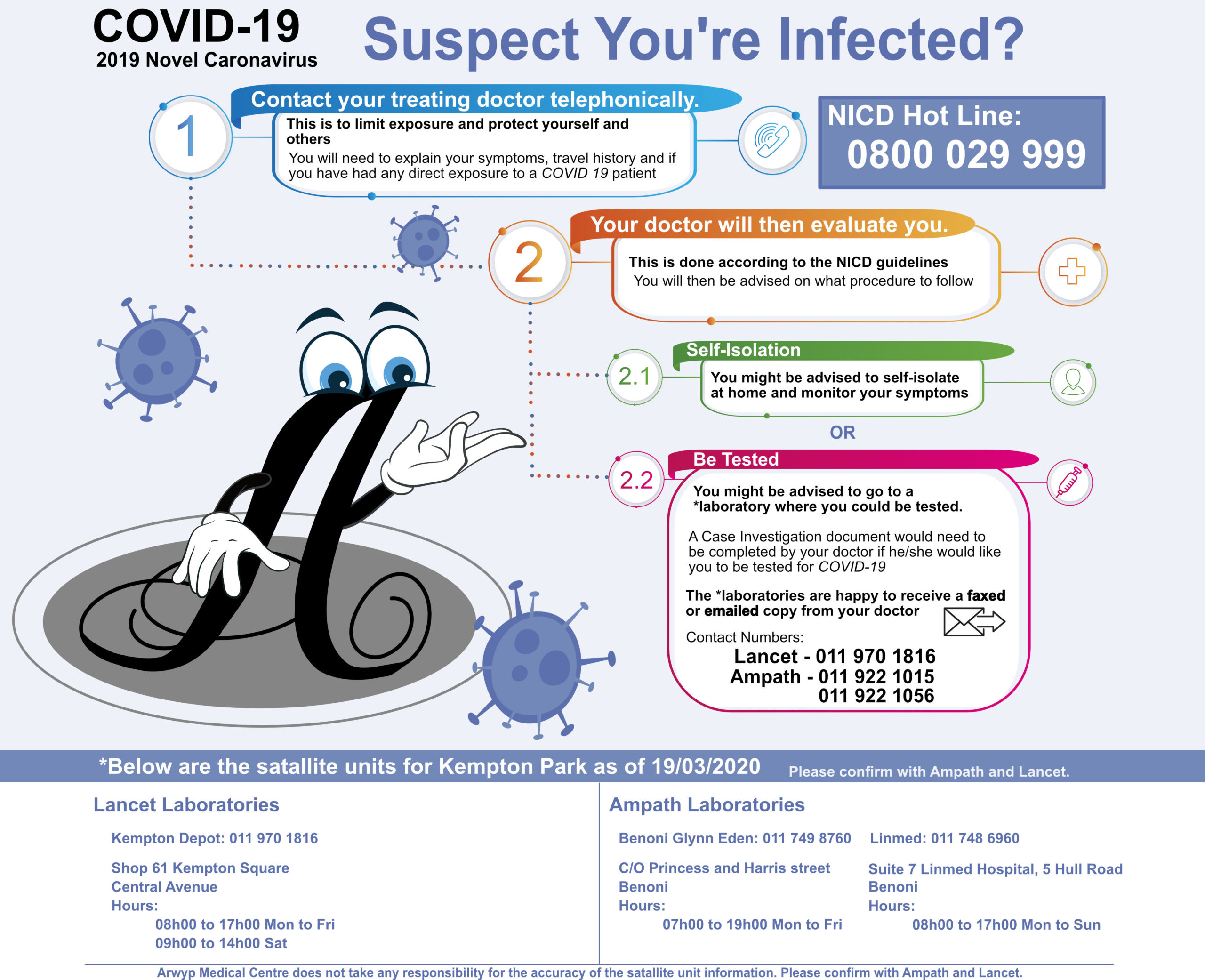
A patient who suffered haemorrhagic stroke needs to be seen at the emergency unit.